Normal Swallowing
Swallowing is a complex process that involves many muscles within the mouth, throat and esophagus. Normal swallowing involves four phases, including the oral preparatory, oral, pharyngeal and esophageal phases. The oral preparatory phase involves preparing the liquids and food to be swallowed. This phase includes chewing and manipulation of the food and liquids. During the oral phase, the tongue propels the food and liquid into the oropharynx (or back of the throat), at which point a swallow should trigger. Once the swallow triggers, a complex series of neuromuscular events occur which assist in propelling the food and liquid through the pharynx (or throat) into the esophagus. These events also prevent material from entering the nose and the trachea (or airway). The esophageal phase involves propulsion of the liquids or food through the esophagus into the stomach.
Swallowing Impairment after Head and Neck Treatment
Dysphagia, or difficulty swallowing, can occur after treatment for head and neck cancer. Swallowing problems can include difficulty manipulating liquids or food within the mouth, difficulty chewing, foods and liquids entering the nose, difficulty propelling liquids or foods into the pharynx, difficulty triggering a swallow, trouble clearing foods and liquids through the pharynx into the esophagus and difficulty with clearance of food through the esophagus. Aspiration, or entry of liquids and foods into the airway, can also occur with dysphagia. Patients who undergo surgery for tumors of the oral cavity, oropharynx, larynx, and nasopharynx may have difficulty swallowing after surgery. Those who undergo chemoradiotherapy for treatment of head and neck cancer can also develop problems swallowing, as the muscles involved can become less flexible. For patients who require surgery, the head and neck reconstructive surgeon attempts to reconstruct the surgical defect with swallow function in mind.
Rehabilitative Solutions
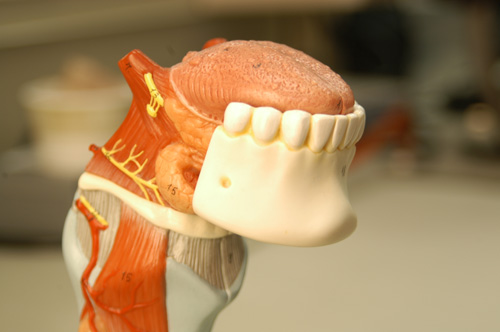
Swallowing rehabilitation focuses on improving swallow efficiency and safety. Swallowing rehabilitation can include: 1) use of head postures to modify the flow of material through the oral cavity and pharynx; 2) swallow maneuvers, which alter the swallow physiology to improve timing and extent of movement of head and neck structures and result in improved airway protection and clearance of foods and liquids through the oral cavity and pharynx and; 3) modification of the type, amount and texture of liquids and foods, to improve swallow safety (i.e., elimination of aspiration) and efficiency through the oral cavity and pharynx. An initial clinical and/or instrumental assessment of swallowing will determine the type of treatment needed, as well as type of diet. Prosthetic management can also improve swallow ability in those patients who have undergone surgery on the tongue, palate or mandible (jaw). Palatal augmentation prostheses can improve tongue-palate contact to help move foods and liquids through the mouth after tongue surgery and palatal obturators can improve resonance (reduce hypernasality) and reduce the risk of foods and liquids entering the nasal cavity after surgery. Mandibular surgical reconstruction and prosthetics can improve cosmesis as well as chewing ability.
Rehabilitative Decision Making
A multidisciplinary team can most effectively assess, manage and treat patients who experience dysphagia after head and neck cancer treatment. The head and neck reconstructive surgeon, speech pathologist, and maxillofacial prosthodontist, should be consulted to evaluate the need for clinical and instrumental assessment of swallowing and determine the need for and appropriate prosthetic management.
