Functional Problem
Tumors of the palate and maxillary sinus often require the removal of the bone of the palate as well as the orbital rim and orbital floor in select clinical situations. The removal of those supporting structures can cause several functional problems for the patient. The upper teeth are supported by the alveolar process of the maxilla and must be removed in most instances of palatomaxillary resections. Support for the eye is dependent on the bone of the orbital floor. Midface projection that provides symmetry with the other side is also dependent on the infrastructure provided by the malar eminence, also known as the cheek bone. Certain aspects of the normal vocal quality are also adversely affected when there is a communication between the mouth and the nose or sinuses, leading to an escape of air that is readily apparent during normal conversational speech.
Rehabilitative Solutions
Priorities in rehabilitating palatomaxillary defects are to achieve an air tight and water tight seal between the oral cavity and the maxillary and nasal sinuses. Support for the eye is critical in order to prevent orbital dystopia (an inferior and posterior displacement of the eye). Restoring dentition to the palate is a priority in order to preserve the ability of the patient to effectively masticate (chew) so that he or she can maintain a normal diet. Finally, midface projection should be restored in order to achieve facial symmetry.
There are 2 primary options for rehabilitation of these defects and the particular aspects of each clinical situation will determine which option is best for any given patient. The biology (aggressiveness) of the patient’s tumor and the need for radiation will influence the decision making process. The extent of the defect will also impact on the optimal solution. Other factors such as the quality and stability of the remaining palatal teeth and the manual dexterity of the patient will play a role in the determination as to how best to proceed.
The first option is the use of a maxillary prosthesis which is fabricated by a maxillofacial prosthodontist. This appliance offers several advantages. In particular it provides teeth over the missing segment of the palate and provides a barrier between the mouth and the nose and sinuses. These palatal prostheses are usually quite bulky, but do not extend superiorly enough to provide support for the globe or augmentation of the cheek for facial symmetry. In individuals with a small oral opening due to radiation or surgery (trismus), or in individuals with impaired manual dexterity, the use of a prosthesis will be prohibitive. The stability and retention of a prosthesis is dependent on a number of factors, but in general, the larger the defect and the poorer the quality of the remaining teeth, then the selection of a prosthetic solution will be less satisfactory. Following radiation to the mouth, the prosthesis tends to place significant stress on the remaining teeth which can become more problematic as time passes following that treatment.
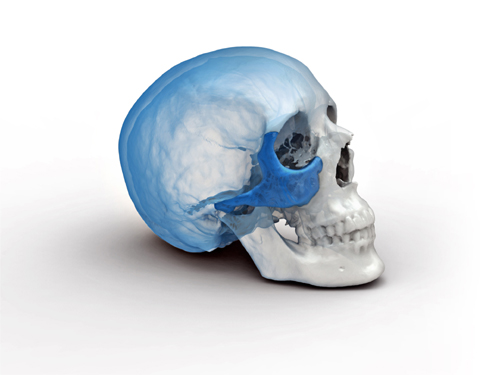
The second option for rehabilitation is one that has emerged over the past decade and has gained more widespread acceptance. The reconstruction of the palatomaxillary defect with native tissue provides a permanent seal between the oral cavity and the nose and sinuses. A variety of reconstructive options have been applied to accomplish the goals listed above. For smaller defects of the palate, a local flap known as the palatal island flap can be applied. Free flaps that are transferred from other parts of the body have been widely used for reconstruction of a variety of defects in the head and neck following cancer surgery. These flaps allow the transfer of native tissue with an artery and vein that must be anastomosed (attached by performing microsurgery) to an artery and vein in the head and neck in order to restore the circulation to that tissue and to permit that flap to heal to the surrounding tissues. The radial forearm flap can be used for limited defects of the palate that are too large for a palatal island flap. When the hemipalate must be reconstructed, then bone from either the fibula (one of the 2 bones in the lower leg) or the iliac crest (hip bone) has been successfully utilized. The fibula is more often used when the defect is limited to the palate and does not extend upwards to the orbit. Alternatively when the defect does extend to involve the orbit, then the iliac crest provides a solution for restoration of the inferior orbital rim, the orbital floor and the malar eminence. Both the fibula and the iliac crest provide healthy bone into which dental implants can be placed to permit dental rehabilitation to occur. With the benefit of dental implants, either a fixed denture, or a removal denture can be created that provides the most stable form of dental restoration. The technical demands of reconstructing the midface region using these techniques are significant and only a few centers in the world have the expertise required to perform this surgery successfully.
Rehabilitative Decision Making
The patient who is facing surgery for a palatal or a maxillary tumor (benign or malignant) should consult with both a head and neck reconstructive surgeon and a maxillofacial prosthodontist in order to have a discussion as to which of these 2 options is best for them. Patients who have undergone a previous resection (tumor removal) and who have a prosthesis in place that they are dissatisfied with, should undergo a consultation with an experienced reconstructive team in order to better understand the pros and cons of a secondary reconstruction of their particular defect.
